| Chapter 1: | The Patient Interview | |
| Page 1 0f 3 |
| This informative and valuable module reviews the skills utilized in pulmonary patient assessment, including: patient interview techniques, observation and physical examination procedures, medical records evaluation, and interpretation of diagnostic test results. The emphasis is on techniques for identifying the signs and symptoms relevant to the patientís pulmonary condition. Accurate assessments lead to prescription of appropriate and effective respiratory care protocols. | 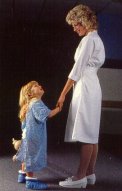 |
Introduction
The "interview" takes place at the very beginning of the relationship with patients. The practitioner simply proceeds to ask the patient about the nature of their problems or complaints. This patient interview can reveal important information relating to symptoms, the patientís emotional/mental state, and their own perception of the problem. The interview is where questions regarding complaints of cough and dyspnea are clarified. Signs of distress in the interview include: the patient sitting forward or in a braced position, anxious or fearful facial expressions, rapid respiratory rates, and interrupted speech patterns.
The purposes of the initial patient interview are to establish rapport, identify the functional status of patient, elicit assessment data, and introduce therapy. Youíve probably heard it said that "how" you say something is often as important as "what" you say. In that vein, before we discuss the types of questions you should ask during the initial patient interview, letís review interviewing techniques and how to structure the interview.
A basic but important aspect of interviewing involves the RCP being able to convey genuine concern for the patientís well-being. Empathy towards the patient can be expressed in several ways. For example, establishing good eye contact during the interview not only lets patients know you are interested in what they are saying, but helps the RCP control the interview.
Patients can easily sense when a practitioner is just "doing their job" and has no sincere interest in their problems. Clinicians who have this approach not only "turn off" the patient, but also frequently overlook potentially significant information. As a result, their assessment of the patient is incomplete, inaccurate, and often leads to the prescription of inappropriate or unnecessary treatments.
Another way RCPs can convey their genuine concern for patientsí condition involves "how" they ask questions during the interview. Posing questions that can be answered with a simple "yes" or "no" is usually inappropriate, counter-productive, and fails to encourage productive communications. An interview that employs more open-ended questions calling for extended responses encourages the patient to "open-up" and reveal information that facilitates an accurate patient assessment. When appropriate, the use of touch may also be an effective means of demonstrating empathy during an interview.
Interview Structure
To ensure success, even the briefest of patient assessment interviews needs to have a pre-established structure. The nature and content of the questions that will be asked during the interview require an environment that is private and quiet in order to encourage honest and effective communications.
Prior to entering the patientís room, you should organize your thoughts so that youíre ready to ask appropriate questions that will enable you to obtain pertinent clinical information. If youíre well organized, youíll be able to avoid repeating questions and wonít forget to ask key questions. Whenever possible, the setting for the interview should allow for a face-to-face conversation. You should begin the interview by addressing the patient by name, introducing yourself, and explaining your role and the purpose of the interview. This should start the process of putting the patient at ease regarding what is going on.
During the interview, be sure to observe the patient closely and listen carefully to what they have to say so you can identify their mood, level of intelligence, and general state of well-being. Acutely ill or apparently anxious patients may need some reassurances prior to starting in-depth questioning.