| Course |
· COPD prevalence and morbidity data that are available probably greatly underestimate the total burden of the disease because it is not usually recognized and diagnosed until it is clinically apparent and moderately advanced.
· Prevalence, morbidity, and mortality vary appreciably across countries, but in all countries where data are available COPD is a significant health problem in both men and women.
· The substantial increase in the global burden of COPD projected over the next twenty years reflects, in large part, the increasing use of tobacco worldwide, and the changing age structure of populations in developing countries.
· Medical expenditures for treating COPD and the indirect costs of morbidity can represent a substantial economic and social burden for societies and public and private payers worldwide. Nevertheless, very little economic information concerning COPD is available.
COPD is a leading cause of morbidity and mortality worldwide and results in an economic and social burden that is both substantial and increasing. COPD prevalence, morbidity, and mortality vary appreciably across countries and across different groups within countries, but in general are directly related to the prevalence of tobacco smoking. Most epidemiological studies have found that COPD prevalence, morbidity, and mortality have increased over time and are greater in men than in women. Very few studies have quantified the economic and social burden of COPD. In developed countries, the direct medical costs of COPD are substantial because the disease is both chronic and highly prevalent. In developing countries, the indirect cost of COPD from loss of work and productivity may be more important than the direct costs of medical care.
Most of the information available on COPD prevalence, morbidity, and mortality comes from developed countries. Even in these countries, accurate epidemiological data on COPD are difficult and expensive to collect. Prevalence and morbidity data greatly underestimate the total burden of COPD because the disease is usually not diagnosed until it is clinically apparent and moderately advanced. The imprecise and variable definitions of COPD have made it hard to quantify the morbidity and mortality of this disease in developed1 and developing countries. Mortality data also underestimate COPD as a cause of death because the disease is more likely to be cited as a contributory than as an underlying cause of death, or may not be cited at all2.
Available estimates of COPD prevalence have been developed by determining either the proportion of the population that reports having respiratory symptoms and/or airflow limitation, or the proportion that reports having been diagnosed with COPD, chronic bronchitis, or emphysema by a physician. Each of these approaches will yield a different estimate, and may be useful for different purposes. For example, studies that ask about the full range of COPD symptoms from early to advanced disease are useful to estimate the total societal burden of the disease. Data on doctor diagnoses of COPD are useful to estimate the prevalence of clinically significant disease that is of sufficient severity to require health services, and therefore is likely to incur significant costs.
The population surveys necessary to develop accurate estimates of COPD prevalence are costly to do and therefore have not been conducted in many countries. Obtaining reliable prevalence data for COPD in each country should be a priority in order to alert those responsible for planning prevention services and healthcare delivery to the high prevalence and cost of the disease. The prevalence of COPD is likely to vary appreciably depending on the prevalence of risk factor exposure, age distribution, and prevalence of susceptibility genes in different countries.
Until recently, virtually all population-based studies in developed countries showed a markedly greater prevalence and mortality of COPD among men compared to women3-6. Gender-related differences in exposure to risk factors, mostly cigarette smoking, probably explain this pattern. In developing countries, some studies report a slightly higher prevalence of COPD in women than men. This likely reflects exposure to indoor air pollution from cooking and heating fuels (greater among women) as well as exposure to tobacco smoke (greater among men)7-15. Recent large population-based studies in the US show a different pattern emerging, with the prevalence of COPD almost equal in men and women16,17. This likely reflects the changing pattern of exposure to the most important risk factor, tobacco smoke.
Estimates based on self-report of respiratory symptoms. COPD prevalence data based on self-report of respiratory symptoms (chronic cough, sputum production, wheezing, and shortness of breath) include people at risk for COPD (Stage 0) as well as those with airflow limitation, and thus yield maximum prevalence estimates. These studies reveal sizable variations in the prevalence of respiratory symptoms depending on smoking status, age, occupational and environmental exposures, country or region, and, to a lesser extent, gender and race. The data also reveal appreciable variations over time, reflecting important temporal changes in populations’ exposure to risk factors such as smoking, outdoor air pollution, and occupational exposures.
The third National Health and Nutrition Examination Survey (NHANES 3)16, a large national survey conducted in the US between 1988 and 1994, included self-report questions about respiratory symptoms. The prevalence of respiratory symptoms varied markedly by smoking status (current>ex>never). Among white males, chronic cough was reported by 24% of smokers, 4.7% of ex-smokers, and 4.0% of never smokers. The prevalence of chronic cough among white women was 20.6% in smokers, 6.5% in ex-smokers, and 5.0% in never smokers. There was a smaller gradient in the prevalence of chronic cough by race (white>black). The prevalence of sputum production was similar to that of chronic cough in these groups.
Estimates based on the presence of airflow limitation. People may have respiratory symptoms such as cough and sputum production for many years before developing airflow limitation. Thus, COPD prevalence data based on the presence of airflow limitation provide a more accurate estimate of the burden of COPD that is, or probably soon will be, clinically significant. However, the use of different cut points to define airflow limitation makes comparing the results of different studies difficult.
In the NHANES 3 study16, airflow limitation was defined as an FEV1/FVC < 70%. The prevalence of airflow limitation was lower than the prevalence of respiratory symptoms found in the same study, but both sets of data reinforce the view that smoking is the most important determinant of COPD prevalence in developed countries. Among white males, airflow limitation was present in 14.2% of current smokers, 6.9% of ex-smokers, and 3.3% of never smokers. Among white females, the prevalence of airflow limitation was 13.6% in smokers, 6.8% in ex-smokers, and 3.1% in never smokers. Airflow limitation was more common among white smokers than among black smokers.
Estimates based on physician diagnosis of COPD. COPD prevalence data based on physician diagnosis provide information about the prevalence of clinically significant COPD that is of sufficient severity to prompt a visit to a physician. Few population-based prevalence surveys have been published to provide this information, and available data are often confusing because asthma and COPD diagnoses are not separated, all age groups are considered together, or chronic bronchitis and emphysema are considered separately.
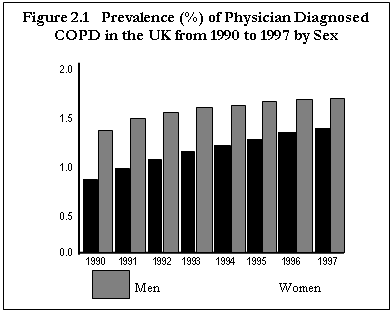
In the UK the General Practice Research Database18, which is based on 525 practices serving 3.4 million patients (6.4% of the total population of England and Wales), provides population-based data on physician-diagnosed COPD (Figure 2-1). In 1997, the prevalence of COPD was 1.7% among men and 1.4% among women. Between 1990 and 1997, the prevalence increased by 25% in men and 69% in women. The prevalence of COPD among men plateaued in the mid-1990s, but continued to increase among women, reaching in 1997 the level observed in men in 1990. The General Practice Research Database includes all ages and thus underestimates the true impact of COPD on older adults.
 |
The Global Burden of Disease Study. The WHO/World Bank Global Burden of Disease Study19,20 used data from both published and unpublished studies to estimate the prevalence of various diseases in different countries and regions around the world (Figure 2-2). Where few data for a region were available, experts made informed estimates. Where no information was available, preliminary estimates were derived from data from other regions that were believed to have similar epidemiological patterns. Using this approach, the worldwide prevalence of COPD in 1990 was estimated at 9.34/1,000 in men and 7.33/1,000 in women. However, these estimates include all ages and underestimate the true prevalence of COPD in older adults.
Figure 2.2 COPD Around the World (All Ages)
|
Region or Country |
1990 Prevalence per 1,000 Males/Females |
|
Established Market Economies |
6.98/3.79 |
|
Formerly Socialist Economies of Europe |
7.35/3.45 |
|
India |
4.38/3.44 |
|
China |
26.2/23.7 |
|
Other Asia and Islands |
2.83/1.79 |
|
Sub-Saharan Africa |
4.41/2.49 |
|
Latin America and Caribbean |
3.36/2.72 |
|
Middle Eastern Crescent |
2.69/2.83 |
|
World |
9.34/7.33 |
Given the striking dearth of population-based data on COPD prevalence in many countries of the world, the values listed in Figure 2-2 should not be viewed as very precise. Nevertheless, some general patterns emerge. The prevalence of COPD is highest in countries where cigarette smoking has been, or still is, very common, while the prevalence is lowest in countries where smoking is less common, or total tobacco consumption per capita is still low. The lowest COPD prevalence among men (2.69/1,000) was found in the Middle Eastern Crescent (a group of 36 countries in North Africa and the Middle East) and the lowest prevalence among women (1.79/1,000) was found in the region referred to as “Other Asia and Islands” (a group of 49 countries and islands, the largest of which is Indonesia and which includes Papua New Guinea, Nepal, Vietnam, Korea, Hong Kong, and many small island countries). Except in the Middle Eastern Crescent, the prevalence of COPD is higher among men than among women.
The Global Burden of Disease study reported a significantly higher prevalence of COPD in China than in most of the other regions (26.20/1,000 among men and 23.70/1,000 among women). A more recent survey conducted in three regions of China (Northern: Beijing; Northeast: Liao-Ning; and South-Mid: HuBei) in persons older than 15 years estimated the prevalence of COPD at 4.21/1,000 among men and 1.84/1,000 among women21.
Morbidity includes physician visits, emergency department visits, and hospitalizations. COPD databases for these outcome parameters are less readily available and usually less reliable than mortality databases. The limited data available indicate that morbidity due to COPD increases with age and is greater in men than women17,22,23.
In the UK, general practice consultations for COPD during one year ranged from 4.17/1,000 in 45- to 64-year-olds to 8.86/1,000 in 65- to 74-year-olds to 10.32/1,000 in 75- to 84-year-olds. These rates are 2 to 4 times the equivalent rates for chest pain due to ischemic heart disease24.
In 1994, according to statistics from the UK Office of National Statistics25, there were 203,193 hospital admissions in Northern Ireland, Scotland, Wales, and England for COPD; the average length of hospital stay among those admitted for a COPD diagnosis was 9.9 days.
US data indicate that in 1997 there were 16.365 million (60.6/1,000) ambulatory care visits for COPD and 448,000 (1.66/1,000) hospitalizations for which COPD was the first-listed discharge diagnosis23. Hospitalization rates for COPD increased with age and were higher among men than among women. These data should be interpreted cautiously, however, because the ICD-9 codes for COPD that were in use in 1997, 490-492 and 494-496, include “bronchitis not specified as acute or chronic.” Therefore, the data for ambulatory care visits are likely to have been inflated by inclusion of visits for acute bronchitis16.
Of all of the descriptive epidemiological data for COPD, mortality data are the most readily available, and probably the most reliable. (The World Health Organization publishes mortality statistics for selected causes of death annually for all WHO regions26; additional information is available from the WHO Evidence for Health Policy Department27.) However, inconsistent use of terminology for COPD causes problems that do not arise for many other diseases. For example, prior to about 1968 and the Eighth Revision of the ICD, the terms “chronic bronchitis” and “emphysema” were used extensively. During the 1970s, the term “COPD” increasingly replaced those terms in the US and some but not all other countries, making comparisons of COPD mortality in different countries very difficult. However, the situation has improved with the Ninth and Tenth Revisions of the ICD, in which deaths from COPD or chronic airways obstruction are included in the broad category of “COPD and allied conditions” (ICD-9 codes 490-496 and ICD-10 codes J42-46).
The age-adjusted death rates for COPD by race and sex in the US from 1960 to 1996 by ICD code are shown in Figure 2-317. COPD death rates are very low among people under age 45 in the US, but then increase with age, and COPD becomes the fourth or fifth leading cause of death among those over 4517, a pattern that reflects the cumulative effect of cigarette smoking28. Although appreciable variations in mortality across developed countries for both genders have been reported29, these differences should be interpreted cautiously. Differences between countries in death certification, diagnostic practices, the structure of healthcare systems, and life expectancy have an appreciable impact on reported mortality rates.
Figure 2.3
Rate 100,000 Population
Because COPD is highly prevalent and can be severely disabling, direct medical expenditures and the indirect costs of morbidity and premature mortality from COPD can represent a substantial economic and social burden for societies and public and private insurance payers worldwide. Nevertheless, very little quantitative information concerning the economic and social burden of COPD is available in the literature today.
Cost of illness studies provide insight into the economic impact of a disease. Some countries attempt to separate economic burden into disease-attributable direct and indirect costs. The direct cost is the value of healthcare resources devoted to diagnosis and medical management of the disease. Indirect costs reflect the monetary consequences of disability, missed work and school, premature mortality, and caregiver or family costs resulting from the illness. Data on these topics from developing countries are not available, but data from the US and some European countries provide an understanding of the economic burden of COPD in developed countries.
United States. Figure 2-4 compares the estimated costs of various lung disorders in the US in 1993. In 1993, the annual economic burden of COPD in the US was estimated at $23.9 billion17, including $14.7 billion in direct expenditures for medical care services, $4.7 billion in indirect morbidity costs, and $4.5 billion in indirect costs related to premature mortality. With an estimated 15.7 million cases of COPD in the US30, the estimated direct cost of COPD is $1,522 per COPD patient per year.
Figure 2.4
Direct and Indirect Costs of Lung Diseases, 1993 (US$ Billions)
|
Condition |
Total Cost |
Direct Medical Cost |
Mortality-Related Indirect Cost |
Morbidity-Related Indirect Cost |
Total Indirect Cost |
COPD |
23.9 |
14.7 |
4.5 |
4.7 |
9.2 |
|
Asthma |
12.6 |
9.8 |
0.9 |
0.9 |
2.8 |
|
Influenza |
14.6 |
1.4 |
0.1 |
13.1 |
13.2 |
|
Pneumonia |
7.8 |
1.7 |
4.6 |
1.5 |
6.1 |
|
Tuberculosis |
1.1 |
0.7 |
--. |
-- |
0.4 |
|
Lung Cancer |
25.1 |
5.1 |
17.1 |
2.9 |
20.0 |
In a US study31 of COPD-related illness costs based on the 1987 National Medical Expenditure Survey, per capita expenditures for inpatient hospitalizations of COPD patients ($5,409 per hospitalization) were 2.7 times the expenditures for patients without COPD ($2,001 per hospitalization). In 1992, under Medicare, the US government health insurance program for individuals over 65, annual per capita expenditures for people with COPD ($8,482) were nearly 2.5 times higher than annual expenditures for people without COPD ($3,511)32.
United Kingdom. In 1996, the direct cost of COPD in the UK was approximately £846 million (about US $1.393 billion) or £1,154 (about US $1,900) per person per year, according to data from the National Health Service (NHS) Executive33. Pharmaceutical expenditures for COPD and allied conditions accounted for 11.0% of the total expenditures for prescription medications Only 2% of total primary care expenditures were for COPD-related visits.
In 1996, lost work productivity, disability, and premature mortality from COPD in the UK accounted for an estimated 24 million days of work lost. The indirect cost of the disease was estimated at £600 million (about US $960 million) for attendance and disability living allowance and £1.5 billion (about US $2.4 billion) to employers for work absence and reduced productivity24.
The Netherlands. In 1993, the direct cost of COPD in the Netherlands was estimated to exceed US $256 million, or US $813 per patient per year. Assuming constant costs and treatment patterns, the direct cost is expected to reach US $410 million per year by 2010. In 1993 inpatient hospitalizations accounted for 57% of the total direct cost of COPD, and medications accounted for an additional 23%. The indirect cost of COPD in the Netherlands was not available34.
Sweden. The direct cost of COPD-related medical care in Sweden was estimated at 1.085 billion SEK (about US $179.4 million) in 1991. The estimated indirect cost of COPD was an additional 1.699 billion SEK (about US $280.8 million)35.
Comparison of different countries. Figure 2-5 provides data on the economic burden of COPD in four countries with Western styles of medical practice and social or private insurance structures. The data are standardized to equivalent year on a per capita basis. After adjusting to a common base year and population, the costs of COPD were relatively similar. The remaining variability in across-country estimates of economic burden can be partly explained by several factors, including: disease prevalence and demographics, particularly smoking patterns; the type and usage patterns of healthcare and non-healthcare services among patients with COPD; the relative prices of healthcare services; employment and wage rates; and the availability of medical prevention strategies and treatments for COPD. Similar data from developing countries are not available.
|
Figure 2.5 Four-Country Comparison of COPD Direct and Indirect Costs |
|||||
|
Country (ref) |
Year |
Direct Cost (US$ M) |
(US$ M) Indirect Cost |
Total (US$ M) |
Per Capita* (US$) |
|
UK33 |
1996 |
778 |
3,312 |
4,090 |
65 |
|
Netherlands34 |
1993 |
256 |
N/A |
N/A |
N/A# |
|
Sweden35 |
1991 |
179 |
281 |
460 |
60 |
|
US1 |
1993 |
14,700 |
9,200 |
23,900 |
87 |
|
* Per capita valuation based on 1993 population estimates from the United Nations Population Council and expressed in 1993 US dollars. # The authors did not provide estimates of indirect costs. |
|||||
Home care. Individuals with COPD frequently receive professional medical care in their homes. In some countries, national health insurance plans provide coverage for oxygen therapy, visiting nursing services, rehabilitation, and even mechanical ventilation in the home, although coverage for specific services varies from country to country36.
Any estimate of direct medical expenditures for home care under-represents the true cost of home care to society, because it ignores the economic value of the care provided to those with COPD by family members. In developing countries especially, direct medical costs may be less important than the impact of COPD on workplace and home productivity. Because the healthcare sector might not provide long-term supportive care services for severely disabled individuals, COPD may force two individuals to leave the workplace - the affected individual and a family member who must now stay home to care for the disabled relative. Since human capital is often the most important national asset for developing countries, COPD may represent a serious threat to their economies.
Since mortality offers a limited perspective on the human burden of a disease, it is desirable to find other measures of disease burden that are consistent and measurable across nations. The World Bank/WHO Global Burden of Disease Study19 designed a method to estimate the fraction of mortality and disability attributable to major diseases and injuries using a composite measure of the burden of each health problem, the Disability-Adjusted Life Year (DALY). The DALYs for a specific condition are the sum of years lost because of premature mortality and years of life lived with disability, adjusted for the severity of disability.
The leading causes of DALYs lost worldwide in 1990 and 2020 (projected) are shown in Figure 2-6. In 1990, COPD was the twelfth leading cause of DALYs lost in the world, responsible for 2.1% of the total. According to the projections, COPD will be the fifth leading cause of DALYs lost worldwide in 2020, behind ischemic heart disease, major depression, traffic accidents, and cerebrovascular disease. This substantial increase in the global burden of COPD projected over the next twenty years reflects, in large part, the increasing use of tobacco worldwide and the changing age structure of populations in developing countries.
|
Figure 2.6 - Leading Causes of Disability-Adjusted Life Years (DALYs) Lost Worldwide: 1990 and 2020 (Projected)2,32 |
|
||||
|
Disease or Injury |
Rank 1990 |
% of Total DALYs |
Rank 2020 |
% of Total DALYs |
|
|
Lower respiratory infections |
1 |
8.2 |
6 |
3.1 |
|
|
Diarrheal diseases |
2 |
7.2 |
9 |
2.7 |
|
|
Perinatal period conditions |
3 |
6.7 |
11 |
2.5 |
|
|
Unipolar major depression |
4 |
3.7 |
2 |
5.7 |
|
|
Ischemic heart disease |
5 |
3.4 |
1 |
5.9 |
|
|
Cerebrovascular disease |
6 |
2.8 |
4 |
4.4 |
|
|
Tuberculosis |
7 |
2.8 |
7 |
3.1 |
|
|
Measles |
8 |
2.6 |
25 |
1.1 |
|
|
Road traffic accidents |
9 |
2.5 |
3 |
5.1 |
|
|
Congenital anomalies |
10 |
2.4 |
13 |
2.2 |
|
|
Malaria |
11 |
2.3 |
19 |
1.5 |
|
|
COPD |
12 |
2.1 |
5 |
4.1 |
|
|
Trachea, bronchus, lung cancer |
33 |
0.6 |
15 |
1.8 |
|
|
Excerpted with permission from Murray CJL, Lopez AD. Science 1999; 274:740-3. Copyright 1999 American Association for the Advancement of Science |
|||||
1. Pride NB, Vermeire P, Allegra L. Diagnostic labels applied to model case histories of chronic airflow obstruction. Responses to a questionnaire in 11 North American and Western European countries. Eur Respir J 1989; 2:702-9.
2. Mannino DM, Brown C, Giovino GA. Obstructive lung disease deaths in the United States from 1979 through 1993. An analysis using multiple-cause mortality data. Am J Respir Crit Care Med 1997; 156:814-8.
3. Buist AS, Vollmer WM. Smoking and other risk factors. In: Murray JF, Nadel JA, eds. Textbook of respiratory medicine. Philadelphia: WB Saunders Co.; 1994. p. 1259-87.
4. Thom TJ. International comparisons in COPD mortality. Am Rev Respir Dis 1989; 140:S27-34.
5. Xu X, Weiss ST, Rijcken B, Schouten JP. Smoking, changes in smoking habits, and rate of decline in FEV1: new insight into gender differences. Eur Respir J 1994; 7:1056-61.
6. Feinleib M, Rosenberg HM, Collins JG, Delozier JE, Pokras R, Chevarley FM. Trends in COPD morbidity and mortality in the United States. Am Rev Respir Dis 1989; 140:S9-18.
7. Chen JC, Mannino MD. Worldwide epidemiology of chronic obstructive pulmonary disease. Current Opinion in Pulmonary Medicine 1999; 5:93-9.
8. Dossing M, Khan J, al-Rabiah F. Risk factors for chronic obstructive lung disease in Saudi Arabia. Respiratory Med 1994; 88:519-22.
9. Dennis R, Maldonado D, Norman S, Baena E, Martinez G. Woodsmoke exposure and risk for obstructive airways disease among women. Chest 1996; 109:115-9.
10. Perez-Padilla R, Regalado U, Vedal S, Pare P, Chapela R, Sansores R, et al. Exposure to biomass smoke and chronic airway disease in Mexican women. Am J Respir Crit Care Med 1996; 154:701-6.
11. Behera D, Jindal SK. Respiratory symptoms in Indian women using domestic cooking fuels. Chest 1991; 100:385-8.
12. Amoli K. Bronchopulmonary disease in Iranian housewives chronically exposed to indoor smoke. Eur Respir J 1998; 11:659-63.
13. Pandey MR. Prevalence of chronic bronchitis in a rural community of the Hill Region of Nepal. Thorax 1984; 39:331-6.
14. Pandey MR. Domestic smoke pollution and chronic bronchitis in a rural community of the Hill Region of Nepal. Thorax 1984; 39:337-9.
15. Samet JM, Marbury M, Spengler J. Health effects and sources of indoor air pollution. Am Rev Respir Dis 1987; 136:1486-508.
16. National Center for Health Statistics. Current estimates from the National Health Interview Survey, United States, 1995. Washington, DC: Department of Health and Human Services, Public Health Service, Vital and Health Statistics; 1995. Publication No. 96-1527.
17. National Heart, Lung, and Blood Institute. Morbidity & mortality: chartbook on cardiovascular, lung, and blood diseases. Bethesda, MD: US Department of Health and Human Services, Public Health Service, National Institutes of Health; 1998. Available from: URL: www.nhlbi.nih.gov/nhlbi/seiin/other/cht-book/htm
18. Soriano JR, Maier WC, Egger P, Visick G, Thakrar B, Sykes J, et al. Recent trends in physician diagnosed COPD in women and men in the UK. Thorax 2000; 55:789-94.
19. Murray CJL, Lopez AD. Evidence-based health policy - lessons from the Global Burden of Disease Study. Science 1996; 274:740-3.
20. Murray CJL, Lopez AD, eds. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Cambridge, MA: Harvard University Press; 1996.
21. Xian Sheng Chen. Analysis of basic data of the study on prevention and treatment of COPD. Chin J Tuber Respiratory Dis 1998; 21:749-52 (with English abstract).
22. Higgins MW, Thom T. Incidence, prevalence, and mortality: intra- and inter-country differences. In: Hensley M, Saunders N, eds. Clinical epidemiology of chronic obstructive pulmonary disease. New York: Marcel Dekker.; 1989. p. 23-43.
23. National Center for Health Statistics. National hospital interview survey. Vital and health statistics, series 10 (issues from 1974 to 1995).
24. Calverley PMA. Chronic obstructive pulmonary disease: the key facts. London: British Lung Foundation; 1998.
25. Office of National Statistics. Mortality statistics (revised) 1994, England and Wales. London: Her Majesty’s Stationery Office; 1996.
26. World Health Organization. World health statistics annual 1995. Geneva: World Health Organization; 1995.
27. World Health Organization, Geneva. Available from: URL: www.who.int
28. Renzetti AD, McClement JH, Litt BD. The Veterans Administration Cooperative Study of Pulmonary Function. III: Mortality in relation to respiratory function in chronic obstructive pulmonary disease. Am J Med 1966; 41:115-29.
29. Incalzi RA, Fuso L, De Rosa M, Forastiere F, Rapiti E, Nardecchia B, et al. Co-morbidity contributes to predict mortality of patients with chronic obstructive pulmonary disease. Eur Respir J1997; 10:2794-800.
30. Singh GK, Matthews TJ, Clarke SC. Annual summary of births, marriages, divorces, and deaths: United States, 1994. Monthly Vital Statistics Report 14 (13). National Center for Health Statistics, Hyattsville, MD.
31. Sullivan SD, Strassels S, Smith DH. Characterization of the incidence and cost of COPD in the US. Eur Respir J 1996; 9:S421.
32. Grasso ME, Weller WE, Shaffer TJ, Diette GB, Anderson GF. Capitation, managed care, and chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998; 158:133-8.
33. National Health Service Executive. Burdens of disease: a discussion document. London: Department of Health; 1996.
34. Rutten-van Molken MP, Postma MJ, Joore MA, Van Genugten ML, Leidl R, Jager JC. Current and future medical costs of asthma and chronic obstructive pulmonary disease in the Netherlands. Respir Med 1999; 93:779-87.
35. Jacobson L, Hertzman P, Lofdahl C-G, Skoogh B-E, Lindgren B. The economic impact of asthma and COPD in Sweden 1980 and 1991. Respir Med 2000; 94:247-55.
36. Fauroux B, Howard P, Muir JF. Home treatment for chronic respiratory insufficiency: the situation in Europe in 1992. The European Working Group on Home Treatment for Chronic Respiratory Insufficiency. Eur Respir J 1994; 7:1721-6.
| Course |