| Note: if you have not officially enrolled in this course and want to get CEU credit, please enroll here: http://www.ceu.org/enroll.html. Without this enrollment, the credits cannot be sent to your state board for licensure. |
|
Introduction (Remember to bookmark this page into Favorites) |
|
The American Lung Association and the World Health Organization track respiratory disease and mortality rates related to tobacco use—in particular COPD—and according to their latest reports:
United States - Approximately 16.4 million people suffer from this disease. According to the American Lung Association, approximately 14 million people suffer from chronic bronchitis, the seventh leading chronic condition in the United States. There are an estimated 1.9 million people suffering with emphysema. Of these, 55.5% are men and 44.5% are women. Between 1982 and 1995 emphysema increased in women by 14.8%, probably due to the increased rate of smoking among women. An estimated 50,000 to 100,000 people, primarily of northern European descent, have AAT deficiency emphysema. COPD is the fourth leading cause of death in the United States. In 1996, approximately 100,360 people died as a result of COPD.
Russian Federation - Tobacco is a major cause of male mortality in the Russian Federation. In 1995, 280,000 people died from tobacco use. Tobacco caused approximately one-third of all male deaths in 1995 and 18% of all deaths. Three-fourths of those men were under 70 years of age.
United Kingdom and Northern Ireland - Although tobacco use has declined dramatically in the U.K., the death rate attributable to COPD and tobacco use was 63 per 100,000 men and 25.1 per 100,000 women in the early 1990s.
China - According to the WHO, tobacco consumption in China doubled between 1965 and 1990. In the mid-1990s, smoking caused far more deaths from COPD than from cardiovascular disease. China has the world’s highest rate of mortality attributable to tobacco use.
Airway obstruction is a common cause of cardiopulmonary disease, and the obstructions can occur either in the upper or lower airways. The primary causes of these obstructions are mucosal edema, bronchial spasm, increased secretions, and bronchiolar collapse. Chronic bronchitis and emphysema are associated with lower airway obstructions. The most common cause of obstruction is the term COPD in which exhalation is impeded. In COPD patients, normal passive exhalation cannot overcome the high expiratory flow resistance and exhalation often requires strenuous muscular efforts. Muscle fatigue can result, leading to hypercapnia, respiratory acidosis, and respiratory failure.
Smoking tobacco causes 80% to 90% of COPD cases. An agent in tobacco smoke stimulates inflammation in the lungs, leading to destruction of the alveoli and narrowing of the airways. While smoking is related to most cases of emphysema, only 15% to 20% of smokers develop the disease. What other factors contribute to the development of “smokers emphysema” remains unclear.
Familial emphysema, or alpha1-antitrypsin (AAT) deficiency-related emphysema, is caused by the hereditary deficiency of a protein called alpha1-antitrypsin. This deficiency leads to uncontrolled destruction of the alveoli and emphysema. Occupational exposure to dust, fumes, and gases appears to contribute slightly to lung function decline and chronic bronchitis. The role of air pollution in COPD remains controversial
Chronic obstructive pulmonary disease (COPD) is an extremely imprecise term used to describe a wide variety of chronic respiratory conditions. In this CEU, the acronym COPD is used to refer to chronic bronchitis and emphysema, although much of the information is equally applicable to other conditions such as asthma, cystic fibrosis, and bronchiolitis.
According to Eric J. Cassell, author of The Nature of Suffering and the Goals of Medicine, the term COPD represents an example of the failure of classical structural disease concepts. He writes that the term COPD has come to replace the structural diagnoses of emphysema and chronic bronchitis.
According to Cassell, “Epidemiologists in the United States and Great Britain could not find structural changes in the lungs that were consistently associated with functional impairment in breathing common to patients in England and America. They ended up agreeing on the definition of the condition to be called chronic obstructive pulmonary disease: the disease present in a patient who coughed and brought up phlegm for as much as three months a year for at least two years! No such definition previously existed in modern medicine. Chronic obstructive pulmonary disease (COPD) is a reduction in the ability to breathe (characterized by certain sharply defined abnormalities in the physiologic measurement of the breathing function) that occurs in the presence of various structural changes—there is no unique alteration in structure.”
He suggests that the motivation for arriving at a name for this complex of pulmonary ailments was that “patients generally expect structural disease names as a diagnosis for their illnesses” and that they are “encouraged in this expectation by their doctors.” As Cassell explains, the basic problem is that the idea of structure, while it may have some “everyday utility” is that is an artificial idea. “Structure is what you see under a microscope. Structure is what pathologists tell us about. (Which is why disease theory made the pathologists the referee of medicine.) But what you see under the microscope is not what is happening in sick people. Nothing in nature holds still like that--everything is changing all the time. what we call function merely changes fast enough for us to measure it in a clinical setting. Even the structure of the body changes constantly,” Cassell concludes.
Nevertheless, the term COPD is very much alive and well among respiratory caregivers. Regardless of the type or degree of underlying pathology, all COPD patients demonstrate several common characteristics:
· chronically increased airway resistance, resulting in increased work of breathing
· decreased efficiency of inspiratory muscles secondary to chronic thoracic hyperinflation, and
· impaired pulmonary gas exchange due to ventilation-perfusion (V/Q) mismatching and, particularly in emphysema, alveolar-capillary destruction.
There is reason to believe that some of these patients have central ventilatory drive dysfunction resulting in diminished responsiveness to increasing PaCO2 or decreasing partial pressure of oxygen, arterial (PaO2).
Patients with stable COPD often manifest arterial hypoxemia (PaO2 less than 80 mm Hg on room air); however, CO2 retention (compensated respiratory acidosis) is less common. Although CO2 retention is most frequently seen in patients with severe COPD, some retain CO2 with moderate disease while others remain normobaric despite severe airway obstruction.
Some event or series of events, when superimposed on these gas exchange deficiencies, may destabilize this precarious homeostasis, exacerbating the patient’s symptoms and causing clinically significant deterioration. Acute respiratory failure superimposed on chronic respiratory failure is a common challenge faced in critical care medicine. this condition is compatible with arterial blood gas measurements revealing a PaO2 below 55 mm Hg, a PaCO2 above 50 mm Hg, and a pH below 7.35, particularly when concomitant metabolic acidosis has been excluded.
Although acute respiratory failure superimposed on COPD is a catastrophic event, appropriate therapy is often lifesaving. In fact, a 2-year survival as high as 72% may be expected when mechanical ventilation is not required, and there is evidence that these patients actually have a life expectancy comparable to that of stable outpatients with the same severity of COPD who have not experienced acute respiratory failure.
Chronic Obstructive Pulmonary Disease
While airway obstructions can occur in the areas of the trachea and larynx or the lower airways, most focus on obstructive lung disease center around the chronic diseases affecting the lower airways. The most common of these are chronic bronchitis, emphysema, and asthma. While it’s possible for a patient to have predominantly one or the other, most adult patients have a combination of those disorders.
While these combinations of disorders occur so frequently in the patient population that they are referred to as chronic obstructive pulmonary disease, it is important that pulmonary assessments recognize and evaluate the differences. The symptoms of advanced chronic bronchitis (including chronic dyspnea, exercise intolerance and daily productive cough for three months for at least two consecutive years) differ from those of asthma in that they are much less reversible.
The pathophysiology responsible for the symptoms of chronic bronchitis includes mucous gland hypertrophy and hypersecretion, which occurs in response to chronic irritation of the airways, and nearly irreversible decreases in small airway diameter. the hypertrophied mucous glands obstruct airflow in the small airways, and the mucus secretions provide an excellent culture medium for bacteria. In sum, this predisposes patients to both frequent bronchial infections and inadequate ventilation. As the disease progresses, most patients also develop emphysema. After reviewing the following illustrations, you are ready to proceed to the core of this course: the newly released (April 4, 2001) international guidelines for the diagnosis, management, and prevention of Chronic Obstructive Lung Disease (COPD). These comprehensive guidelines provide you with extensive information regarding COPD—ranging from definitions and etiologies to treatment recommendations and suggestions for future research. We hope you will greatly benefit from taking this comprehensive course.
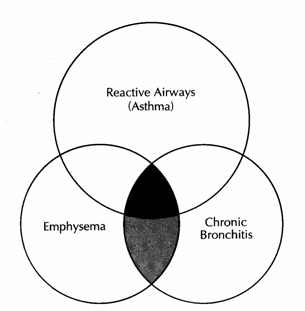
Relationship of asthma, chronic bronchitis, and emphysema as components of chronic obstructive pulmonary disease (COPD).
The exact proportions of overlap between these components is unclear; the diagram is not proportional. Many patients have features of emphysema and chronic bronchitis; as a result of cigarette smoking (lightly shaded area). Hyperreactive airways may be common feature in many subjects who develop chronic bronchitis or emphysema. Some patients may display symptoms of all three disorders (dark shaded areas).
Redrawn from Burrows B, Knudson RJ, and Kettrl LG:
V insufficiency, St Louis, 1975, Mosby.
Human Respiratory System
Global Initiative for Chronic Obstructive Lung Disease (GOLD)
Given the relative confusion and disagreement among healthcare professionals regarding the topic of “COPD,” it was an historic breakthrough that on April 4, 2001, the medical world was greeted with the following important news release:
![]()
FOR IMMEDIATE
RELEASE Contact:
Wednesday, April 4, 2001 NHLBI Communications Office
(301) 496-4236
International Guidelines Released on
Chronic Obstructive Lung Disease (COPD)
Fourth Leading Cause of Death in US and Worldwide
The first international guidelines for the diagnosis, management, and prevention of Chronic Obstructive Lung Disease (COPD) — currently the fourth leading cause of death in the US and worldwide — were released today by an international team of scientists from the Global Initiative for Chronic Obstructive Lung Disease (GOLD). The GOLD Workshop Report, which provides evidence-based recommendations for the clinical management of COPD, is the first step in an international effort to boost awareness of COPD and improve the way it is treated. GOLD was created by the National Heart, Lung, and Blood Institute (NHLBI) at the National Institutes of Health and the World Health Organization.
According to NHLBI Director Dr. Claude Lenfant, “COPD has become a major public health problem worldwide. That’s why we, with the WHO, initiated this program. We hope that this report will increase worldwide awareness of COPD and help the millions of people who suffer from this disease.”
COPD, a term used to describe chronic bronchitis and emphysema, is a slowly progressive airways disease characterized by a gradual loss of lung function. In the US, it is caused primarily by cigarette smoking. There is no known cure, but smoking cessation can slow disease progression.
COPD has been on the increase in the US, and in 1996, an estimated 16 million Americans had COPD. The number of deaths attributed to COPD has also increased substantially in the past 40 years to approximately 100,000 men and women per year in the US alone. The highest rate of increase in deaths has been seen in white women.
It is expected that by 2020, COPD will rank as the third leading cause of death, surpassing stroke. The annual cost of COPD to the US economy is estimated at nearly $30.4 billion.
The GOLD Report, which was reviewed extensively by medical societies in more than 100 countries throughout both the developed and developing world, emphasizes the need for clinicians and patients to recognize cough and sputum production as early signs of possible COPD and calls for the use of spirometry, a simple test of lung function, to confirm the diagnosis. It also provides a general scheme for classifying COPD by severity to help clinicians determine how best to manage the condition. Practical recommendations for reducing risk factors and for managing both stable COPD and exacerbations are also provided.
Said Lenfant, “A concerted effort by government officials, healthcare workers, biomedical researchers, industry, and patients throughout the world is required to improve the way COPD is diagnosed and managed and to increase research into improved treatments and ultimately a cure. This effort has begun with the launch of the GOLD Initiative today.”
![]()
Subsequent to the issuance of this press release, the report itself was made available, and we present the most relevant sections of that report here:
The Report
Preface
Chronic Obstructive Pulmonary Disease (COPD) is a major public health problem. It is the fourth leading cause of chronic morbidity and mortality in the United States1 and is projected to rank fifth in 2020 as a worldwide burden of disease according to a study published by the World Bank/World Health Organization2. Yet, COPD fails to receive adequate attention from the healthcare community and government officials. With these concerns in mind, a committed group of scientists encouraged the US National Heart, Lung, and Blood Institute and the World Health Organization to form the Global Initiative for Chronic Obstructive Lung Disease (GOLD). Among GOLD’s important objectives are to increase awareness of COPD and to help the thousands of people who suffer from this disease and die prematurely from COPD or its complications.
The first step in the GOLD program was to prepare a consensus Workshop Report, Global Strategy for the Diagnosis, Management, and Prevention of COPD. The GOLD Expert Panel, a distinguished group of health professionals from the fields of respiratory medicine, epidemiology, socio-economics, public health, and health education, reviewed existing COPD guidelines, as well as new information on pathogenic mechanisms of COPD as they developed a consensus document. Many recommendations will require additional study and evaluation as the GOLD program is implemented.
A major problem is the incomplete information about the causes and prevalence of COPD, especially in developing countries. While cigarette smoking is a major known risk factor, much remains to be learned about other causes of this disease. The GOLD Initiative will bring COPD to the attention of governments, public health officials, healthcare workers, and the general public, but a concerted effort by all involved in healthcare will be necessary to control this major public health problem.
I would like to acknowledge the dedicated individuals who prepared the Workshop Report and the effective leadership of the Workshop Chair, Professor Romain Pauwels. It is a privilege for the National Heart, Lung, and Blood Institute to serve as one of the cosponsors. We look forward to working with the World Health Organization, and all other interested organizations and individuals, to meet the goals of the GOLD Initiative.
Development of the Workshop Report was supported through educational grants to the Department of Respiratory Diseases of the Ghent University Hospital, Belgium (WHO Collaborating Center for the Management of Asthma and COPD) from ASTA Medica, AstraZeneca, Aventis, Bayer, Boehringer-Ingelheim, Byk Gulden, Chiesi, GlaxoSmithKline, Merck, Sharp & Dohme, Mitsubishi-Tokyo, Nikken Chemicals, Novartis, Schering-Plough, Yamanouchi, and Zambon.
Claude Lenfant, MD
Director
National Heart, Lung, and Blood Institute
References
1. National Heart, Lung, and Blood Institute. Morbidity & mortality : Chartbook on cardiovascular, lung, and blood diseases. Bethesda, MD: US Department of Health and Human Services, Public Health Service, National Institutes of Health; 1998. Available from: URL: www.nhlbi.nih.gov/nhlbi/seiin//other/cht-book/htm
2. Murray CJL, Lopez AD. Evidence-based health policy-lessons from the Global Burden of Disease Study. Science 1996; 274:740-3.
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is a major cause of chronic morbidity and mortality throughout the world. Many people suffer from this disease for years and die prematurely from it or its complications. COPD is currently the fourth leading cause of death in the world1, and further increases in its prevalence and mortality can be predicted in the coming decades2. A unified international effort is needed to reverse these trends.
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) is conducted in collaboration with the US National Heart, Lung, and Blood Institute (NHLBI) and the World Health Organization (WHO). Its goals are to increase awareness of COPD and decrease morbidity and mortality from the disease. GOLD aims to improve prevention and management of COPD through a concerted worldwide effort of people involved in all facets of healthcare and healthcare policy, and to encourage a renewed research interest in this highly prevalent disease.
A nihilistic attitude toward COPD has arisen among some healthcare providers, due to the relatively limited success of primary and secondary prevention (i.e., avoidance of factors that cause COPD or its progression), the prevailing notion that COPD is largely a self-inflicted disease, and disappointment with available treatment options. The GOLD project will work toward combating this nihilistic attitude by disseminating information about available treatments, both pharmacologic and non-pharmacologic.
Tobacco smoking is a major cause of COPD, as well as of many other diseases. A decline in tobacco smoking would result in substantial health benefits and a decrease in the prevalence of COPD and other smoking-related diseases. There is an urgent need for improved strategies to decrease tobacco consumption. However, tobacco smoking is not the only cause of COPD and may not even be the major cause in some parts of the world. Furthermore, not all smokers develop clinically significant COPD, which suggests that additional factors are involved in determining each individual’s susceptibility. Thus, investigation of COPD risk factors and ways to reduce exposure to these factors is also an important area for future research. New research tools have recently revealed that inflammation plays a prominent role in COPD pathogenesis, but this inflammation is different than that involved in asthma. Further study of the molecular and cellular mechanisms involved in COPD pathogenesis should lead to effective treatments that slow or halt the course of the disease.
Gold Workshop Report:
Global Strategy for the Diagnosis, Management and Prevention of COPD
One strategy to help achieve GOLD’s objectives is to provide healthcare workers, healthcare authorities, and the general public with state-of-the-art information about COPD and specific recommendations on the most appropriate management and prevention strategies. The GOLD Workshop Report, Global Strategy for the Diagnosis, Management, and Prevention of COPD, is based on the best-validated current concepts of COPD pathogenesis and the available evidence on the most appropriate management and prevention strategies. The Report has been developed by individuals with expertise in COPD research and patient care and extensively reviewed by many experts and scientific societies. It provides state-of-the-art information about COPD for pulmonary specialists and other interested physicians. The document will also serve as a source for the production of various communications during the implementation of the GOLD program, including a practical guide for primary care physicians and a document for use in developing countries.
The GOLD Report is not intended to be a comprehensive textbook on COPD, but rather to summarize the current state of the field. Each chapter starts with Key Points that crystallize current knowledge. The chapters on the Burden of COPD and Risk Factors demonstrate the global importance of COPD and the various causal factors involved. The chapter on Pathogenesis, Pathology, and Pathophysiology documents the current understanding of, and remaining questions about, the mechanism(s) that lead to COPD, as well as the structural and functional abnormalities of the lungs characteristic of the disease.
A major part of the GOLD Workshop Report is devoted to the clinical Management of COPD and presents a management plan with four components:
1. Assess and Monitor Disease;
2. Reduce Risk Factors;
3. Manage Stable COPD;
4. Manage Acute Exacerbations.
Management recommendations are largely symptom driven and are presented according to the severity of the disease, using a simple classification of severity to facilitate the practical implementation of the available management options. Where appropriate, information about health education for patients is included.
The final chapter identifies critical gaps in knowledge requiring Further Research and provides a summary of proposed directions for the development of new therapeutic approaches.
Methods Used to Develop This Report
In January, 1997, COPD experts from several countries met in Brussels, Belgium to explore the development of a Global Initiative for Chronic Obstructive Lung Disease. Dr. Romain Pauwels served as Chair; representatives of the NHLBI and WHO attended. Participants agreed that the project was timely and important, and recommended the establishment of a panel with expertise on a wide variety of COPD-related topics to prepare an evidence-based document on diagnosis, management, and prevention of COPD. NHLBI and WHO staff, in concert with Dr. Pauwels, identified individuals from many regions of the world to serve on the Expert Panel, which included health professionals in the areas of respiratory medicine, epidemiology, pathology, socio-economics, public health, and health education.
The first step toward developing the Workshop Report was to review the multiple COPD guidelines already published. The NHLBI collected these guidelines and prepared a summary table of similarities and differences between the documents. Where agreement existed, the Expert Panel drew on these existing documents for use in the Workshop Report. Where major differences existed, the Expert Panel agreed to carefully examine the scientific evidence to reach an independent conclusion.
In September, 1997, several members of the Expert Panel met with a consultant to develop a comprehensive set of terms to build a database of COPD literature. The database and a computer program to search the world literature on COPD have been developed, and they will be placed on the Internet and cross-referenced with the Workshop Report to help keep the Report current as new literature is published.
In April, 1998, the NHLBI and WHO cosponsored a workshop to begin the development of the Report. Workshop participants were divided into three groups: definition and natural history, chaired by Dr. Sonia Buist; pathophysiology, risk factors, diagnosis, and classification of severity, chaired by Dr. Leonardo Fabbri; and management, chaired by Dr. Romain Pauwels. A table of contents was developed and writing assignments were made. The Panel agreed that clinical recommendations would require scientific evidence, or would be clearly labeled as “expert opinion.” Each chapter would contain a set of the most current and representative references.
In September, 1998, the Panel met to evaluate its progress. Members reviewed a variety of evidence tables and chose to assign levels of evidence to statements using the system developed by the NHLBI (Figure A). Levels of evidence are assigned to management recommendations where appropriate in Chapter 5, Management of COPD, and are indicated in boldface type enclosed in parentheses after the relevant statement - e.g., (Evidence A). The methodological issues concerning the use of evidence from meta-analyses were carefully considered (e.g., a meta-analysis of a number of smaller studies was considered to be evidence level B)2. The panel met in May, 1999, September, 1999, and May, 2000 in conjunction with meetings of the American Thoracic Society (ATS) and the European Respiratory Society (ERS). Symposia were held at these meetings to present the developing program and to solicit opinion and comments. The meeting in May, 2000 was the final consensus workshop.
After this workshop, the document was submitted for review to individuals and medical societies interested in the management of COPD. The reviewers’ comments were incorporated, as appropriate, into the final document by the Chair in cooperation with members of the Expert Panel. Prior to its release for publication, the Report was reviewed by the NHLBI and the WHO. A workshop was held in September, 2000 to begin implementation of the GOLD program.
Figure A: Description of Levels of Evidence |
||
|
Evidence Category |
Sources of Evidence |
Definition |
A |
Randomized controlled trials (RCTs). Rich body of data. |
Evidence is from endpoints of well-designed RCTs that provide a consistent pattern of findings in the population for which the recommendation is made. Category A requires substantial numbers of studies involving substantial numbers of participants. |
|
B |
Randomized controlled trials (RCTs). Limited body of data. |
Evidence is from endpoints of intervention studies that include only a limited number of RCTs, posthoc or subgroup analysis of patients, or meta-analysis of RCTs. In general, Category B pertains when few randomized trials exist, they are small in size, they were undertaken in a population that differs from the target population of the recommendation, or the results are somewhat inconsistent. |
|
C |
Nonrandomized trials. Observational studies. |
Evidence is from outcomes of uncontrolled or nonrandomized trials or from observational studies. |
|
D |
Panel Consensus Judgment |
This category is used only in cases where the provision of some guidance was deemed valuable but the clinical literature addressing the subject was deemed insufficient to justify placement in one of the other categories. The Panel Consensus is based on clinical experience or knowledge that does not meet the above-listed criteria. |
References
1. World Health Organization. World health report. Geneva: World Health Organization; 2000. Available from: URL: http://www.who.int/whr/2000/en/statistics.htm
2. Murray CJL, Lopez AD. Evidence-based health policy - lessons from the Global Burden of Disease Study. Science 1996; 274:740-
| Introduction |